This is an extremely common dental intervention that aids in the saving of a tooth from extraction, which is otherwise irreversibly damaged or infected. While in most cases root canals are successful, at times they do fail. Therefore, knowledge of the failure rate of root canals and factors contributing to success or failure is important for both patients and dental professionals. This blog post will outline stats, reasons for failure, and ways to improve the success rate related to root canal treatments.
Understanding Root Canal Treatment
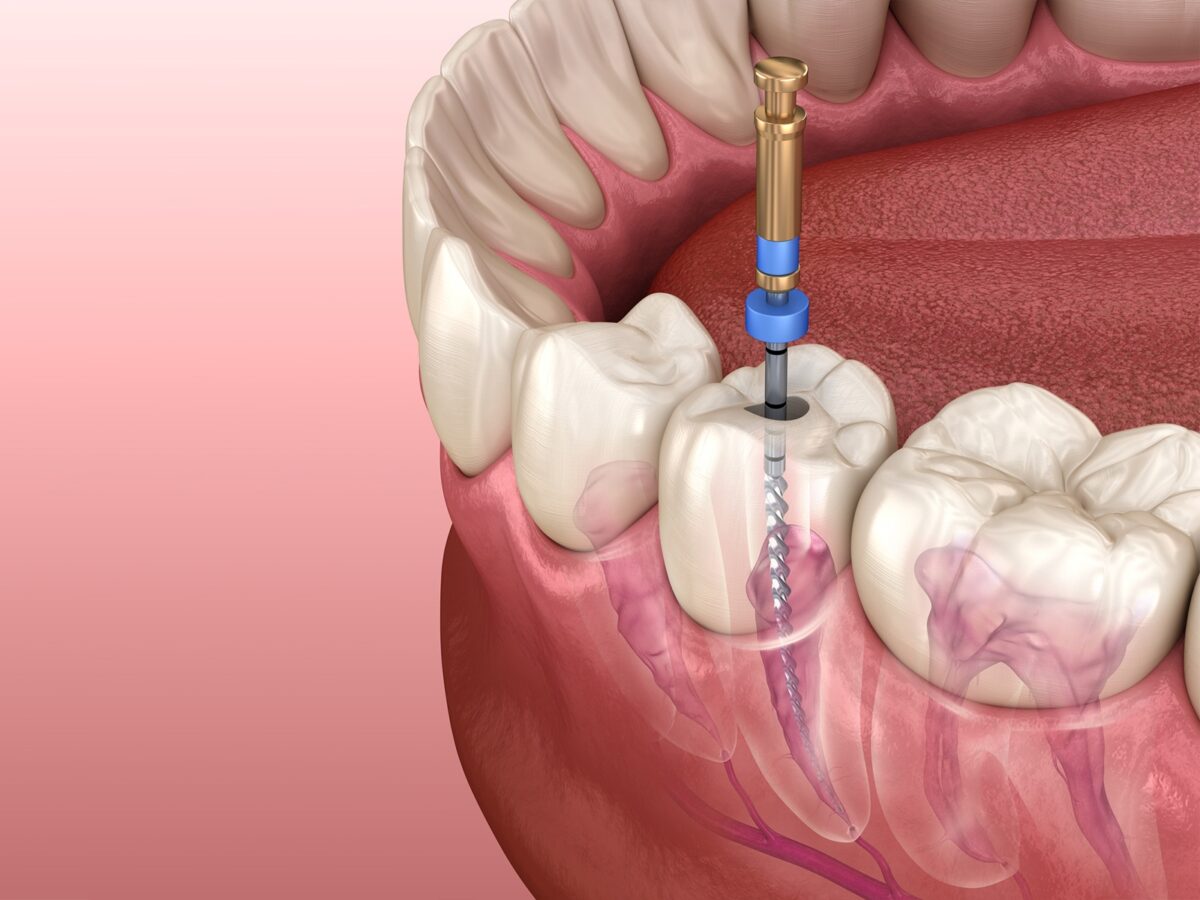
Before discussing the rates of failure, let’s consider exactly what a root canal treatment does. A dentist or an endodontist removes the pulp, infected or damaged, from inside the tooth in this procedure. This is followed by cleaning and shaping the root canals and then filling and sealing them. This aims to eradicate any infection and save the natural tooth structure.
Success Rates of Root Canal Treatments
While not entirely safe, root canal treatments have had some relative success. Several studies and numerous clinical observations show the success rate for initial root canal treatments to be between 85% and 97%. In other words, in the vast majority of cases, root canal treatments do cure dental problems and help patients retain natural teeth for many years.
However, variables that set the results include the case complexity, experience of practitioner, and general oral health of the patient. Success rates are also higher for first-time treatments compared to retreating teeth that have gone through a root canal treatment.
Failure Rates and Their Implications
While the success rates for root canals are outstanding, the other side of the coin should not be ignored – the failure rate. From the success rates given above, it is possible to deduce that the failure rate for root canals will fall between 3% and 15%. That is to say that for every 100 procedures of root canals performed, about 3 through 15 do not end up as desired.
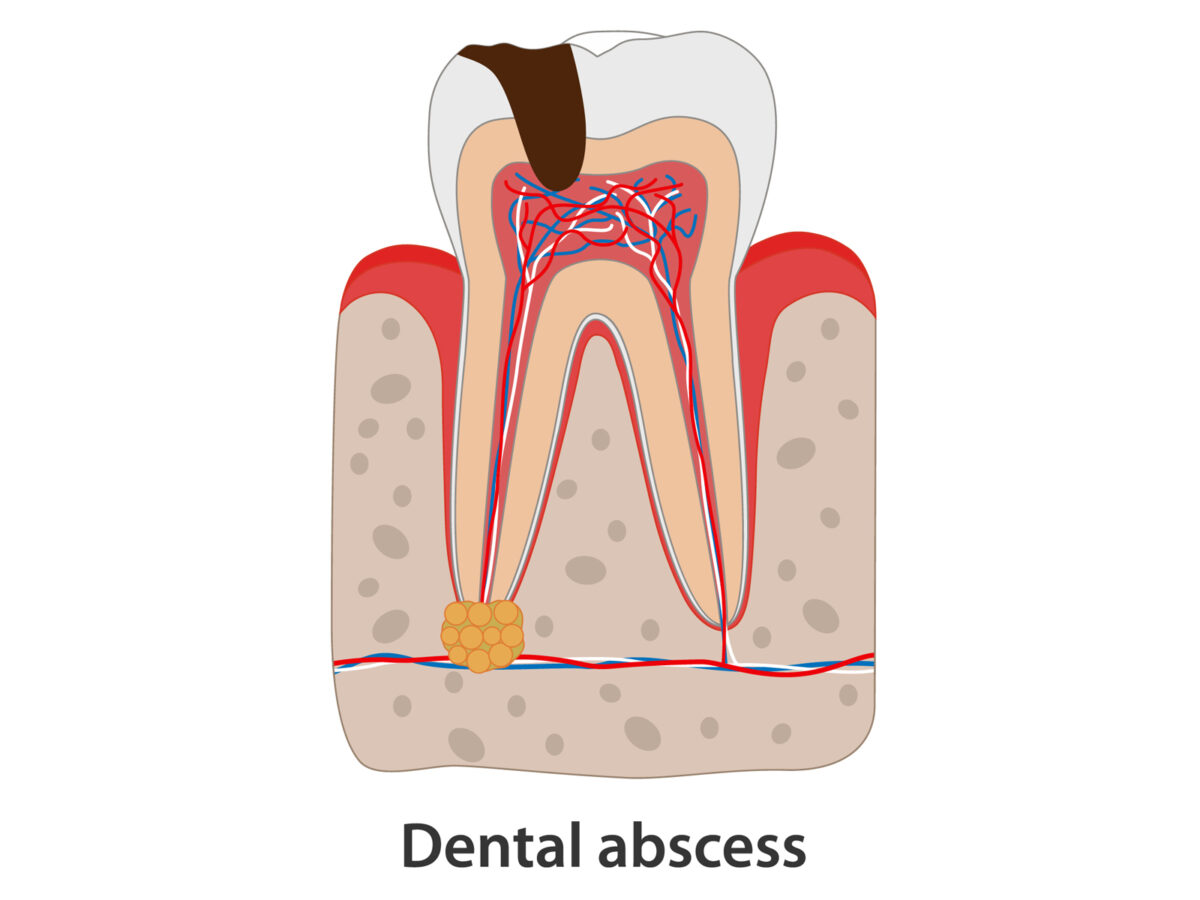
It should be noted that “failure” in the context of root canal treatment does not actually indicate a disaster or immediate problems. In many instances, visible symptoms of a failed root canal appear months to years after the treatment. However, if a root canal has failed, there is a possibility of persistent or recurrent infection and pain, which may require additional dental procedures.
Common Reasons for Root Canal Failure
There are many factors that may cause failure in root canal treatment. To know the reasons will help the dentist and the patient to avoid these pitfalls and take measures to lessen the chances of such failure. Some of the common causes are as follows:
1. Missed canals: Since teeth have complex structures, some teeth have multiple canals. In case the dentist misses any canal, which later turns out to be infected, it will impede healing; hence, treatment will not be successful.
2. Improper cleaning and shaping: The root canals should be cleaned and shaped as such so that all the infected tissue may be removed, rendering the place quite unfavorable for bacterial survival. Anything short of absolute cleaning leads to residual bacteria that reseed and cause reinfection.
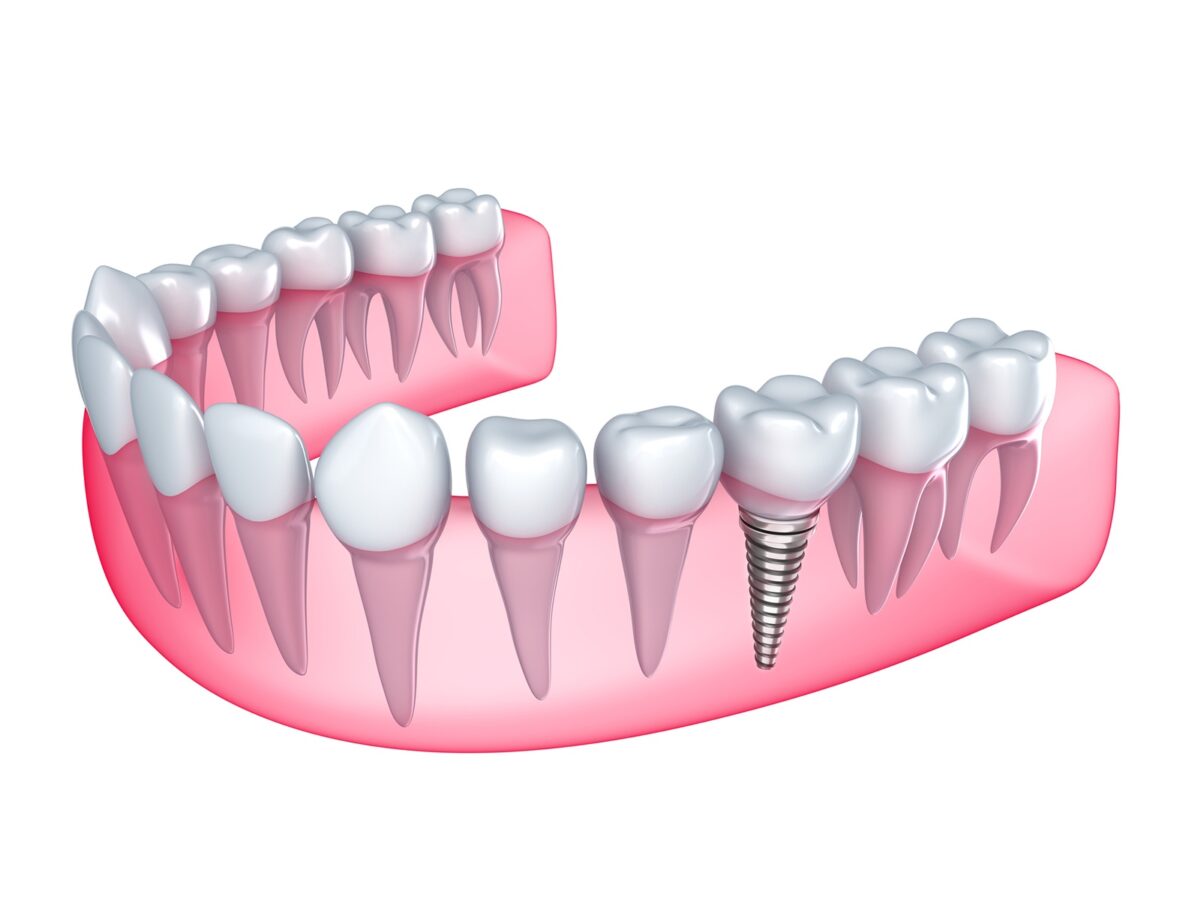
3. Deficient restoration: Proper restoration is required because a tooth is a lot more fragile after a root canal treatment. If the restoration is deemed insufficient, it may contribute to easy access of bacteria to the other parts again, resulting in recontamination and failure.
4. Cracks or fractures: If cracks in the tooth structure are not detected, they may allow entry of bacteria into the tooth and cause reinfection after the root canal is reported to be successful.
5. Resistant bacteria: Sometimes, some bacteria are resistant to otherwise standard modes of treatment and continue causing infection.
6. Systemic factors: Patients with immune-compromised conditions, or with certain systemic diseases, are more likely to have root canal failure because healing is impaired and infection will be more likely to thrive.
Factors That Increase Success and Decrease Failure
Since a root canal treatment involves so many variables, it can never be 100% predictable. However, here are some factors that improve the chances of success and decrease the likelihood of failure:
1. Advanced diagnostic imaging: The availability of improved technologies, such as cone-beam computed tomography (CBCT), enhances the visualization of the root structure and will allow for the recognition of possible complications before the initiation of treatment.
2. Microscope-assisted treatments: Implementation of dental operating microscopes in endodontic therapy enhances visibility—that is, precision—for much more efficient cleaning and treatment of complex canal systems.
3. Proper case selection: Each case is to be assessed regarding the real appropriateness of the root canal and whether some other approaches may be more suitable.
4. Continuing education and training: Dental professionals should keep abreast of the most recent techniques and technologies concerning the practice of endodontics to provide the best possible care.
5. Patient education and follow-up care: Patients should be instructed on the basics of oral hygiene and be scheduled for regular checkups to prevent or detect any further complications at an early stage.
Long-term Follow-up
It is worth noting that the success or failure of a root canal treatment is not always clearly indicated. Some studies have indicated the rates of success to be fairly high in the short term (1-5 years) and drop somewhat in the long term (10+ years). This goes on to indicate the need for ongoing dental care and regular check-ups many years after undergoing a root canal procedure.
So even if the rates for failure in treatments involving root canals are very low, from 3% to 15%, the patient and the professional should never take the complications lightly. From appreciating the factors that contribute to the failure of root canal procedures and implementing some key strategies for success, we should continuously seek further ways to improve this important dental procedure.
It is, therefore, very important that for anyone predisposed to undergo or have undergone root canal treatment, an experienced dental professional should provide the service, post-treatment care guidance should be taken, and regular check-ups be performed. With proper care and attention, the vast majority of root canal treatments can offer long-lasting relief and help preserve natural teeth for years to come.